Diabetes type 2 previously known as Non-Insulin Dependent Diabetes Mellitus is a chronic disorder of metabolism characterise by high blood glucose levels in the body because:
- Your body is not making enough insulin to fulfil its need that is relative insulin deficiency in contrast to the absolute insulin deficiency in type 1 diabetes where the body can’t produce any insulin.
- Your body resists the effects of insulin known as; insulin resistance.
- It could be the combination of the above factors.
Insulin is a very important hormone made by a gland situated below and behind the stomach; the pancreas. Insulin helps and regulates the movement of glucose, the main energy providing fuel of the body, into the cells where it is used to produce energy.
SYMPTOMS
1. Increased Thirst (Polydipsia) With Increased frequency of Micturition; Fluid is pulled out from tissues once you have high sugar levels in your bloodstream making you thirsty. Once you drink more you have to go to the toilet more often.
2. Polyphagia (Increased hunger); As the relative insulin deficiency or the insulin resistance doesn’t allow sugars to enter the cells, the organs and muscles get energy depleted making you more hungry.
3. Weight loss; You eat more because you are more hungry still you lose weight because the energy you are taking is not made available to the cells where it is needed.
4. Fatigue; Energy depleted cells, muscles and organs make you feel tired at all times.
5. Repeated Infections and Poor Healing Wounds.
6. Acanthosis nigrans; some people develop areas of dark pigmented skin on their body especially in the folds and creases.
7. Blurred Vision; In some people high blood sugars may cause water to come out of their lens making it difficult for them to focus.
Apart from the above symptoms many people do not have any symptoms at all and they are diagnosed in a routine clinical evaluation. So these symptoms are very slow to develop and diabetes may be present for a long time before the symptoms develop.
What Puts People At Risk of Developing Type 2 Diabetes
There are many factors that collectively or individually increase the risk of a person developing type 2 diabetes. Some have more influence than the others.
1) Lifestyle; It is one of the most important risk factor for type 2 diabetes. It includes:
a. Obesity; waist line more than 80cm(31.5 inches) in women and more than 94cm(37 inches) in men increases the risk.
b. Lack of physical activity.
c. Poor diet; including excess of sugar sweetened drinks, plenty of white rice, food rich in saturated fats and trans fatty acids.
d. Stress; It may be at work or at home increases the risk.
2) Genetics; It is believed that more than 36 genes have been involved in the development of type 2 diabetes.
3) Family History; Risk is increased if a parent or sibling has type 2 diabetes.
4) Age; It develops mainly in people aged 40 or above but can develop earlier as well but increasing age increases the risk.
5) Race; more common in south Asian and African Caribbean people, develops even earlier than 40 years sometimes.
6) Gestational Diabetes; It adds to the risk of developing full type 2 diabetes.
7) Pre diabetes; when your blood sugar levels are higher than the normal values but not high enough to label type 2 diabetes adds on to the risk.
8) Medical conditions and Medicines: for example
a. Acromegaly
b. Cushing syndrome
c. Pheochromocytoma
d. Hyperthyroidism
e. Drugs containing steroids
f. Beta blockers
g. Thiazides
Also Read: Is it Possible to “Cure” Type 2 Diabetes?
TREATMENT
The treatment of type 2 diabetes involves a multidisciplinary team approach. Although diabetes can’t be cured but can be treated and managed very well. This multidisciplinary team includes a doctor, a nurse, a dietitian, a chiropodist, an optometrist and some other healthcare workers. The treatment can be made simpler if it is divided into smaller steps as follows;
STEP 1: Aiming For Normal Blood Glucose Levels
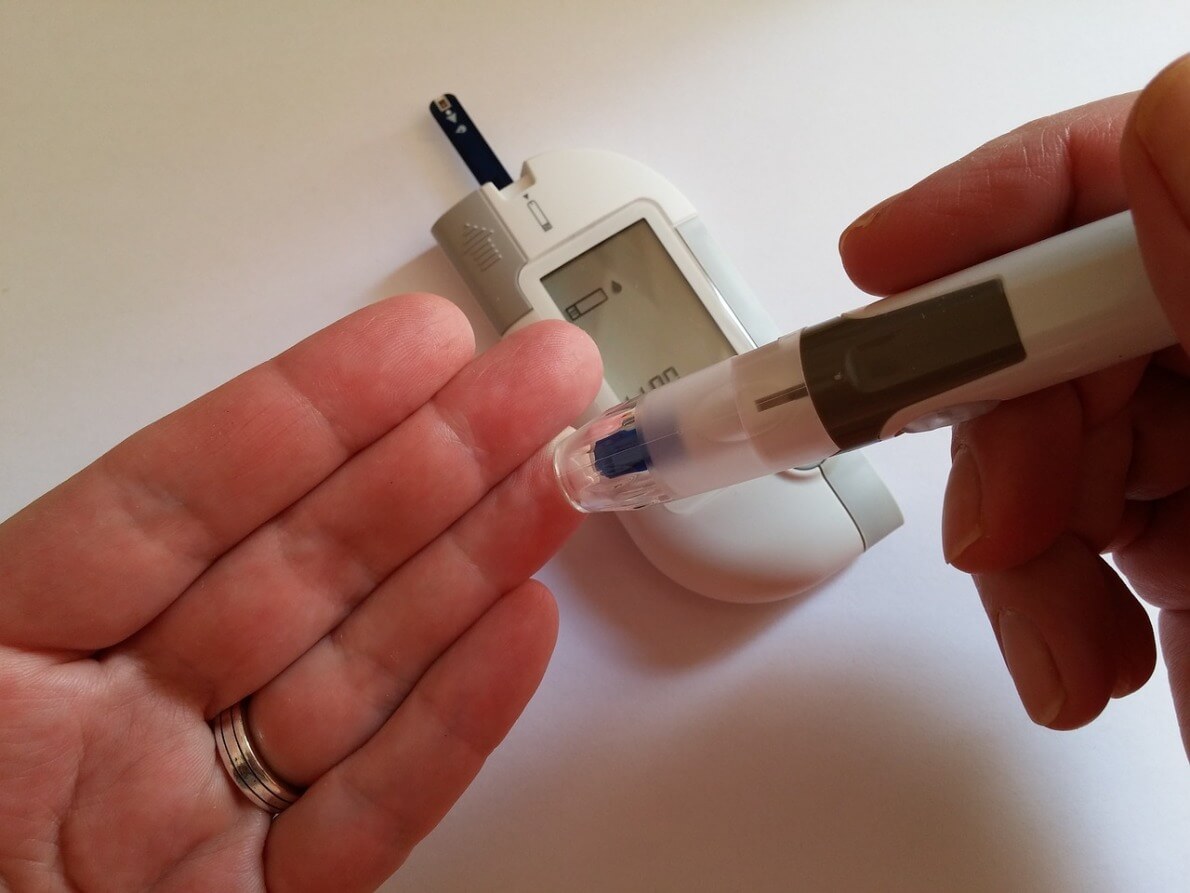
Monitoring Blood Glucose
Your doctor recommends HbA1C test every 2 to 6 months to find out about your average blood glucose levels over the period of time. A target of the levels is also set by your doctor which is usually somewhere between 6.5% to 7.5 %. Treatment modifications can be made according to the levels. You can also monitor your levels regularly with the help of a blood glucose monitor at home and keep a record.
You must be aware that certain conditions alter the blood glucose levels such as Food, Physical activity, Medication, Illness, Stress, Alcohol and Hormones.
Lifestyle Changes
a. Eat Healthy
A healthy diet is a diet low in sugar, salt, fats, high in fibre and has plenty of fruits and vegetables. You and your dietitian can work out a plan that you can easily follow which is according to your food preferences and suits your lifestyle. Once you have your plan you need to be consistent with it.
b. Physical Activity
Physical activity is really important to keep you fit. It helps to lower blood glucose levels. Make sure you know about your blood sugar level before starting an exercise, you may have to take a snack before you start exercising if blood sugar levels are already low. Choose some aerobic exercises first but don’t forget to ask your doctor first before starting any exercise programme especially if you have been inactive for some time. You can choose brisk walking, cycling, swimming, dancing whichever suits your lifestyle. You can gradually build up your routine including stretching and strengthening exercises as well of course after your doctor’s advice .If you can walk briskly for 30 minutes continuously or 2 sessions 15 minutes each at least 5 times a week it is good.
c. Lose weight
If you are overweight it is advisable to lose some weight. It helps to lower blood glucose levels.
These are the simple measures you can take to control your blood glucose levels and for many people they are quite effective. However if the blood glucose levels are still are not under normal range then medicines are used to control the:
Medications
1. Metformin:
Usually this is the first drug given to newly diagnosed diabetics especially who are overweight. It works by lowering the amount of glucose released by the liver in the blood stream plus it makes the cells more responsive to the same level of insulin .Metformin has fewer side effects especially it does not cause hypoglycaemia generally, you may feel sick with mild tummy upset. Side effects can be reduced if the medicine is started from a low dose and gradually build up to the required dose.
2. Sulfonylureas:
Your doctor may add one of these drugs if Metformin alone is not sufficient or you can’t tolerate Metformin due to side effects or you may start off with a Sulfonylurea if you are not overweight. They include: Gliclazide, Glimepiride and Glipizide. These drugs act by enhancing the insulin release from the pancreas and thus can cause hypoglycaemia as a possible complication.
3. Other Drugs:
Thiazolidindiones, Acarbose are some other drugs which your doctor can prescribe if indicated. Every drug has its advantages and side effects, make sure to discuss them with your doctor before you start a therapy.
4. Insulin:
If the blood glucose levels are not controlled by the medications explained above you may have to take insulin injections to control them. There are different types and routes of injecting insulin. Your doctor will recommend the type and the route of injecting insulin that suits you the best. One serious potential complication of insulin is hypoglycaemia.
5. Pregnancy:
Type 2 diabetic women need to alter their treatment regime if they are on oral medicines to control their blood glucose and they will be shifted to insulin throughout their pregnancy.
STEP 2: Reduce Modifiable Risk Factors
You certainly have to cut out or at least reduce the risk factors which you can. They include
1. Stop smoking
2. Lose excess weight if overweight
3. Keep a check on your cholesterol levels; your doctor may prescribe you with a cholesterol lowering medicine known as Statin.
4. Keep your blood pressure under control; you may have to take a medicine to control blood pressure if indicated.
Also Read: Blood Pressure and Weight: Is There a Correlation
STEP 3: Early Detection and Management of Any Complications
It can be achieved only if you keep a regular follow up at a diabetes clinic. A follow up visit will usually include
1. Your blood pressure, blood glucose, HbA1C and serum cholesterol levels check.
2. Healthy lifestyle checks.
3. Advice on foot care.
4. Eye examination to detect any early signs of a developing complication and if so its treatment.
5. Kidney function tests both urine and blood tests to make sure the kidneys are doing fine.
COMPLICATIONS
Short Term Complications;
1. Hyperglycaemia (High blood glucose levels):
It can be caused by overeating, non- compliance with your medicine or illness. Symptoms are fatigue, intense thirst, nausea, frequent urination, dry mouth and blurred vision. If you have some of these symptoms please see your doctor, your diet plan or the medication may have to be adjusted.
2. Hyperosmolar hyperglycaemic Non ketotic syndrome:
A condition characterised by extremely high blood glucose levels may be as high as 600mg/dl (33.3mmol/l) or even more with all the symptoms of hyperglycaemia plus symptoms such as confusion, drowsiness and hallucinations. Seek medical advice promptly.
3. Diabetic Ketoacidosis:
This is a condition more commonly see in untreated type 1 diabetics not common in type 2 diabetics. It is characterise by appetite loss, tummy pain, fatigue, vomiting, weakness and a sweet fruity smell in breath, this is a medical emergency so immediate hospital care is required.
4. Hypoglycaemia:
This is often a complication of treatment diagnosed when the blood glucose gets quite low usually under 4mmol/l. Symptoms are trembling, sweating, anxiety, mood changes, blurred vision, pale appearance, tingling lips and confusion. You can have an attack of hypo if you miss a meal or does some unusual physical activity or you have taken excess of your medication. You should take a sugary drink immediately followed by a sandwich if you think you are having a hypoglycemic episode and check your blood sugar levels after 15 min if still low u can have some more sugary things and recheck after 15 min. Seek medical care if u are becoming drowsy or at least tell someone nearby.
LONG TERM COMPLICATIONS
When blood glucose levels remain high over a long period of time it affects many organs and systems resulting in more chronic difficult to deal with complications. These are
1. Heart and Blood Vessels: can cause heart attacks, angina and stroke.
2. Kidneys: can lead to kidney failure.
3. Eyes: can lead to conditions such as glaucoma, cataracts and even blindness.
4. Nerves: Neuropathies are very common.
5. Combined nerve and vessel problems: Foot problems, Impote the better you manage your diabetes the longer you can delay these long term complications and can achieve better quality of life.
PREVENTION
It is always wise to adapt a healthy lifestyle even if you are not a high risk person to develop type 2 diabetes. A healthy lifestyle includes healthy diet, being physically active and maintaining a normal weight. These measures definitely work in keeping you healthy.
IMMUNISATIONS
Always have your immunisations done against Flu (autumn each year) and against pneumococcal bacteria (once).They help to prevent against the opportunistic infections you may get easily because of your low immunity.